Abstract
Coronary thrombus aspiration during percutaneous coronary intervention (PCI) has been evaluated in numerous studies to determine its effectiveness and safety in patients with acute coronary syndromes, particularly ST-segment elevation myocardial infarction (STEMI). Although thrombus aspiration can improve immediate procedural outcomes by reducing thrombus burden, it does not consistently improve long-term cardiovascular outcomes and is associated with an increased risk of stroke. Consequently, major cardiovascular guidelines generally recommend against routine thrombus aspiration.
Classification of Coronary Thrombus
| Grade | Description | Angiographic Features | Clinical Implications |
| 0 | No Thrombus Visible | Clear coronary arteries without any visible thrombus | Thrombus aspiration generally not indicated |
| I | Possible Thrombus | Hazy or irregular lesion without definite thrombus | Aspiration may not be beneficial; further diagnostic evaluation recommended |
| II | Definite Thrombus, ≤0.5x vessel diameter | Small, well-defined thrombus | Aspiration might be considered; low thrombus burden |
| III | Definite Thrombus, >0.5x vessel diameter | Large thrombus occupying more than half the vessel diameter | Aspiration recommended if associated with significant flow impairment |
| IV | Occlusive Thrombus | Complete vessel occlusion due to thrombus | Aspiration strongly considered to restore flow, especially in STEMI |
| V | Old, Organized Thrombus | Angiographic characteristics of older, fibrotic thrombus | Aspiration less likely to be successful; mechanical intervention or surgery might be required |

Additional Notes:
- Grade I and II thrombi often represent situations where pharmacological therapy with antiplatelet and anticoagulant agents may suffice, reserving mechanical interventions for failure of medical management.
- Grade III and IV thrombi are typically where thrombus aspiration can be most beneficial, especially when combined with stenting and post-dilation to ensure adequate myocardial perfusion.
- Grade V thrombi are challenging due to their older, more organized nature, which makes them resistant to both pharmacological and mechanical interventions.
Procedural Details
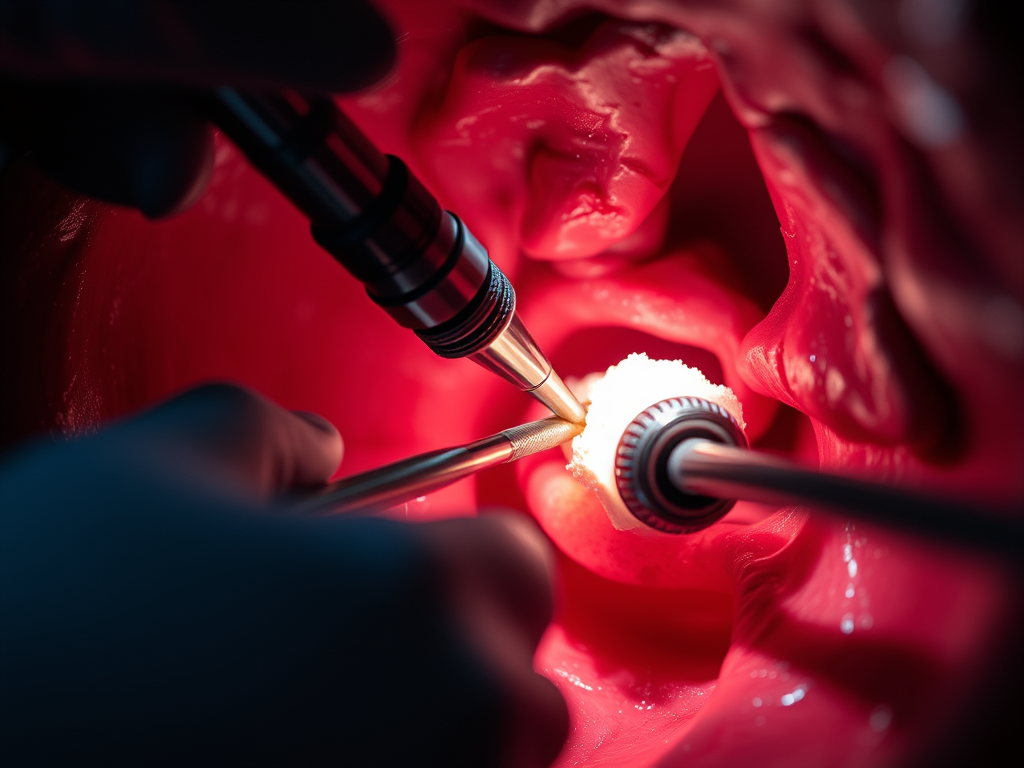
Thrombus aspiration during PCI is performed using a catheter specifically designed to extract thrombus from the coronary arteries. The procedure typically follows these steps:
- Access: Vascular access is obtained, commonly via the radial or femoral artery.
- Catheter Placement: A guide catheter is introduced to the site of the occlusion under fluoroscopic guidance.
- Thrombus Aspiration: An aspiration catheter is advanced through the guide catheter to the thrombus site. The operator then manually aspirates the thrombus by applying suction to the catheter.
- Assessment: After aspiration, angiography is performed to assess flow improvement and ensure no significant residual thrombus is left that might impede flow or cause distal embolization.
- Additional Interventions: Depending on the angiographic result, further interventions such as balloon angioplasty or stent placement may be required to optimize blood flow and support the vessel.
Complications
While thrombus aspiration can be beneficial in selected cases, it carries risks and potential complications, which include:
- Vascular Injury: The catheter can cause damage to the vessel wall, leading to dissections or perforations.
- Distal Embolization: Paradoxically, the procedure intended to prevent distal embolization can itself cause embolization of thrombotic material, leading to new occlusions downstream.
- No-Reflow Phenomenon: Despite successful removal of the thrombus, some patients may experience insufficient reperfusion due to microvascular damage or persistent blockage.
- Stroke: Aspiration can dislodge material that may travel to the cerebral circulation, leading to ischemic strokes.
- Bleeding and Access Site Complications: These are common with any invasive cardiovascular procedure, especially if anticoagulation or antiplatelet therapies are used aggressively.
Indications for Thrombus Aspiration
| Patient Condition | Indication for Thrombus Aspiration | Guideline Recommendation | Level of Evidence |
| STEMI with Visible High Thrombus Burden | Considered in cases where the thrombus burden is likely to impede stent delivery or result in significant distal embolization | Class IIb (Selective Use) | C-LD |
| STEMI without High Thrombus Burden | Not recommended due to lack of demonstrated benefit on mortality and increased risk of stroke | Class III (No Benefit) | A |
| Non-STEMI with Thrombus-Containing Lesions | Not recommended as routine practice; may be considered on a case-by-case basis in specific clinical scenarios | Class III (No Benefit) | A |
| Unstable Angina with Thrombus-Containing Lesions | Generally not recommended; limited data available | No specific recommendations | – |
| Failed Initial PCI Attempt due to Thrombus | May be considered as a bailout strategy to achieve reperfusion if initial PCI does not improve flow due to obstructive thrombus | Class IIb (Selective/Bailout Use) | C-LD |
Results from Major Trials and Meta-Analyses
- TAPAS, TASTE, and TOTAL Trials: These trials indicated no significant benefit in reducing death or major adverse cardiovascular events (MACE) from routine thrombus aspiration in STEMI patients, with some trials suggesting an increased risk of stroke.
- Patient-level Meta-analysis: A comprehensive analysis found no overall benefit in clinical outcomes with routine thrombectomy, although subgroups with high thrombus burden showed a potential reduction in cardiovascular death at the cost of increased stroke risk.
Guideline Recommendations
- American College of Cardiology/American Heart Association (ACC/AHA):
- STEMI: Class III (no benefit) for routine aspiration.
- Selective Use: Class IIb; not well established.
- European Society of Cardiology (ESC): Similar recommendations, emphasizing no routine use.
- Japanese Cardiological Society: Offers a more lenient recommendation for selective use in primary PCI.
Table 1: Summary of Guideline Recommendations
| Condition | Guideline | Recommendation | Class of Recommendation | Level of Evidence |
| STEMI | ACC/AHA, ESC, JCS | Routine aspiration not recommended | III | A |
| Non-STEMI and Unstable Angina | No specific recommendations | – | – | – |
Conclusions
Thrombus aspiration should not be performed routinely in patients undergoing PCI for STEMI due to lack of mortality benefit and increased stroke risk. Selective use may be considered in high thrombus burden cases, but careful patient selection and technique are critical to avoid adverse outcomes.
Bibliography
- Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM, Bittl JA, Cohen MG, DiMaio JM, Don CW, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e4–e17. doi: 10.1161/CIR.0000000000001039
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with st-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393
- Kimura K, Kimura T, Ishihara M, Nakagawa Y, Nakao K, Miyauchi K, Sakamoto T, Tsujita K, Hagiwara N, Miyazaki S, et al. JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ J. 2019;83:1085–1196. doi: 10.1253/circj.CJ-19-0133
- Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the society for cardiovascular angiography and interventions. Circulation. 2016;133:1135–1147. doi: 10.1161/CIR.0000000000000336
- Inohara T, Kohsaka S, Yamaji K, Iida O, Shinke T, Sakakura K, Ishii H, Amano T, Ikari Y. Use of thrombus aspiration for acute coronary syndrome patients: insights from the nationwide percutaneous coronary intervention registry in Japan. J Am Heart Assoc. 2022;11:e025728. doi: 10.1161/JAHA.122.025728
- Kumbhani DJ, Bavry AA, Desai MY, Bangalore S, Bhatt DL. Role of aspiration and mechanical thrombectomy in patients with acute myocardial infarction undergoing primary angioplasty: an updated meta-analysis of randomized trials. J Am Coll Cardiol. 2013;62:1409–1418. doi: 10.1016/j.jacc.2013.04.025
- Frobert O, Lagerqvist B, Olivecrona GK, Omerovic E, Gudnason T, Maeng M, Aasa M, Angeras O, Calais F, Danielewicz M, et al. Thrombus aspiration during ST-segment elevation myocardial infarction. N Engl J Med. 2013;369:1587–1597. doi: 10.1056/NEJMoa1308789
- Lagerqvist B, Frobert O, Olivecrona GK, Gudnason T, Maeng M, Alstrom P, Andersson J, Calais F, Carlsson J, Collste O, et al. Outcomes 1 year after thrombus aspiration for myocardial infarction. N Engl J Med. 2014;371:1111–1120. doi: 10.1056/NEJMoa1405707
- Jolly SS, Cairns JA, Yusuf S, Meeks B, Pogue J, Rokoss MJ, Kedev S, Thabane L, Stankovic G, Moreno R, et al. Randomized trial of primary pci with or without routine manual thrombectomy. N Engl J Med. 2015;372:1389–1398. doi: 10.1056/NEJMoa1415098
- Jolly SS, James S, Dzavik V, Cairns JA, Mahmoud KD, Zijlstra F, Yusuf S, Olivecrona GK, Renlund H, Gao P, et al. Thrombus aspiration in ST-segment-elevation myocardial infarction: an individual patient meta-analysis: thrombectomy trialists collaboration. Circulation. 2017;135:143–152. doi: 10.1161/CIRCULATIONAHA.116.025371
- Taglieri N, Bacchi Reggiani ML, Ghetti G, Saia F, Compagnone M, Lanati G, Di Dio MT, Bruno A, Bruno M, Della Riva D, et al. Efficacy and safety of thrombus aspiration in ST-segment elevation myocardial infarction: an updated systematic review and meta-analysis of randomised clinical trials. Eur Heart J Acute Cardiovasc Care. 2019;8:24–38. doi: 10.1177/2048872618795512
- Secemsky EA, Ferro EG, Rao SV, Kirtane A, Tamez H, Zakroysky P, Wojdyla D, Bradley SM, Cohen DJ, Yeh RW. Association of physician variation in use of manual aspiration thrombectomy with outcomes following primary percutaneous coronary intervention for ST-elevation myocardial infarction: the national cardiovascular data registry CathPCI registry. JAMA Cardiol. 2019;4:110–118. doi: 10.1001/jamacardio.2018.4472
- Thiele H, de Waha S, Zeymer U, Desch S, Scheller B, Lauer B, Geisler T, Gawaz M, Gunkel O, Bruch L, et al. Effect of aspiration thrombectomy on microvascular obstruction in nstemi patients: the TATORT-NSTEMI trial. J Am Coll Cardiol. 2014;64:1117–1124. doi: 10.1016/j.jacc.2014.05.064
- Feistritzer HJ, Meyer-Saraei R, Lober C, Bohm M, Scheller B, Lauer B, Geisler T, Gawaz M, Bruch L, Klein N, et al. Long-term outcome after thrombus aspiration in non-ST-elevation myocardial infarction: results from the TATORT-NSTEMI trial: thrombus aspiration in acute myocardial infarction. Clin Res Cardiol. 2020;109:1223–1231. doi: 10.1007/s00392-020-01613-0