INTRODUCTION
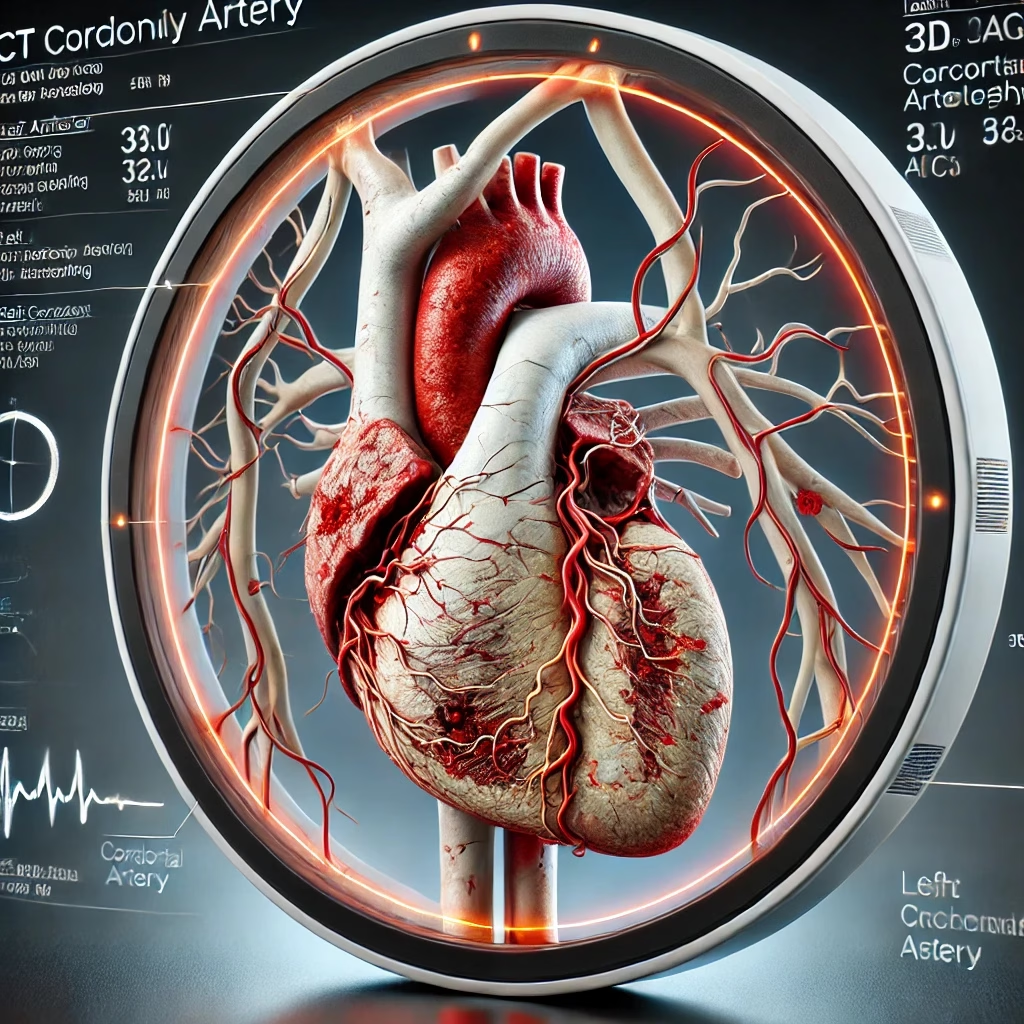
Coronary artery disease (CAD) remains a leading cause of morbidity and mortality worldwide. Timely and accurate diagnosis is critical for effective management and prevention of adverse cardiovascular events. Cardiac computed tomography angiography (CT CAG) has emerged as a non-invasive imaging modality that offers high diagnostic accuracy for detecting coronary artery stenosis and atherosclerosis. With advancements in scanner technology, radiation dose reduction, and integration of artificial intelligence, CT CAG now plays a pivotal role in evaluating patients with suspected CAD.
Table 1: Advantages of CT CAG Over Other Diagnostic Modalities
| Feature | CT CAG | Stress Testing | Invasive Coronary Angiography (ICA) |
| Non-invasiveness | Yes | Yes | No |
| Diagnostic Accuracy | High for stenosis and plaque composition | Moderate for functional ischemia | Gold standard for anatomy |
| Radiation Exposure | Moderate (significantly reduced in newer CTs) | Minimal | Higher than modern CT CAG |
| Risk of Complications | Minimal (contrast nephropathy in rare cases) | Minimal | ~0.1% (stroke, vascular complications) |
| Visualization of Atherosclerosis | Comprehensive (calcified and non-calcified) | Limited | Comprehensive |
| Integration of Functional Data | Possible with FFrCT | Yes | Requires additional testing |
DIAGNOSTIC UTILITY OF CT CAG
CT CAG has revolutionized the non-invasive diagnosis of coronary artery disease (CAD) by offering high sensitivity and specificity for detecting coronary stenosis and plaque characteristics. Compared to invasive coronary angiography (ICA), CT CAG is safer, with no risk of procedural complications, and provides additional insights into atherosclerotic burden beyond stenosis severity.
Key features include:
- High Predictive Values: Positive predictive value (PPV) of CT CAG is high, with an even higher negative predictive value (NPV), making it reliable for ruling out CAD.
- Comprehensive Plaque Characterization: Differentiation between calcified, non-calcified, and mixed plaques aids in risk stratification.
- Pre-Procedural Planning: Facilitates catheter selection and intervention strategies in patients requiring ICA.
CT CAG is particularly valuable in low-to-intermediate-risk patients, reducing unnecessary ICAs and optimizing patient management pathways. It has demonstrated superior accuracy compared to stress testing for anatomical assessment of coronary arteries.
Table 2: Diagnostic Accuracy of CT CAG vs Other Modalities
| Feature | CT CAG | Stress Testing | ICA |
| Sensitivity for CAD | 95-98% | 70-80% | 100% (gold standard) |
| Specificity for CAD | 80-85% | 70-80% | 100% |
| Visualization of Plaque Composition | Yes | No | Limited |
| Procedural Risk | Minimal | Minimal | ~0.1% complication rate |
CT CAG’s ability to integrate functional and anatomical data through fractional flow reserve computed tomography (FFrCT) further enhances its diagnostic utility.
CT CALCIUM SCORING
Coronary artery calcium (CAC) scoring is an integral part of cardiac CT, often used as a preliminary tool to assess the extent of calcification in coronary arteries. It serves as a gatekeeper for performing CT CAG in low-risk populations and provides valuable prognostic information regarding cardiovascular events.
Key points:
- Risk Stratification: A CAC score of 0 is associated with a very low risk of obstructive coronary artery disease (CAD) and future cardiovascular events, allowing for safe deferral of further testing in many cases.
- Relationship with Disease Severity: Higher CAC scores correlate with increased atherosclerotic burden and higher event rates, guiding the need for more aggressive preventive therapies.
- Integration with CT CAG: CAC scoring can be followed by CT CAG in cases where significant calcification is detected, enhancing the detection of both calcified and non-calcified plaques.
Table 3: Interpretation of CAC Scores
| CAC Score | Risk Level | Clinical Implications |
| 0 | Very low risk | No further testing in asymptomatic, low-risk patients |
| 1-99 | Low risk | Initiate lifestyle changes; consider further evaluation |
| 100-399 | Moderate risk | Suggest further diagnostic testing, including CT CAG |
| ≥400 | High risk | Strong indication for CT CAG and potential aggressive therapy |
CAC scoring has been integrated into guideline-directed strategies for managing patients with chest pain, helping to refine clinical decisions regarding further non-invasive or invasive evaluations.
INDICATIONS FOR CT-CAG
Table 4 : Indications for CT CAG with Recommendations
| Clinical Indication | Recommendation | Class/Level of Evidence |
| Stable Chest Pain | First-line test for low-to-intermediate risk patients with suspected coronary artery disease (CAD). | Class I, Level A |
| Acute Chest Pain | Rule out CAD in patients with low-to-intermediate risk presenting to the emergency department. | Class I, Level A |
| Preoperative Coronary Assessment | Evaluation of CAD in patients undergoing non-cardiac high-risk surgeries. | Class IIa, Level B |
| Coronary Anomaly Assessment | Investigation of suspected congenital or acquired coronary artery anomalies. | Class I, Level B |
| Post-CABG Graft Evaluation | Assessment of graft patency in symptomatic or asymptomatic patients post-CABG. | Class IIa, Level B |
| Follow-Up for Stent Patency | Non-invasive evaluation of stent patency in symptomatic patients with prior percutaneous coronary intervention (PCI). | Class IIb, Level B |
| Fractional Flow Reserve CT (FFrCT) | Functional assessment of intermediate stenosis when invasive testing is not feasible or deferred. | Class IIa, Level B |
| Patients with Diabetes or High-Risk CAD | Comprehensive evaluation and risk stratification in patients with diabetes or multi-vessel disease. | Class IIa, Level B |
| Suspected Acute Coronary Syndromes (ACS) | Use in non-ST elevation ACS (NSTEACS) for early detection of obstructive CAD and risk stratification. | Class IIa, Level B |
CORRELATION WITH FUNCTIONAL IMAGING
CT CAG’s integration with functional imaging has enhanced its diagnostic capabilities, particularly through the development of fractional flow reserve computed tomography (FFrCT). This hybrid approach allows for simultaneous anatomical and functional assessment of coronary stenosis, helping to determine its hemodynamic significance.
Key points:
- Fractional Flow Reserve Computed Tomography (FFrCT): Combines anatomical imaging with computational fluid dynamics to estimate blood flow across a stenosis. FFrCT has shown high negative predictive value for ruling out ischemia and avoids the need for invasive pressure wire measurements.
- Comparison with Stress Testing: CT CAG demonstrates superior sensitivity for detecting anatomical stenosis compared to stress testing, while FFrCT provides similar functional insights.
- Integrated Diagnostic Approach: Combining CT CAG with FFrCT reduces unnecessary invasive coronary angiographies and optimizes patient triage.
Table 5: Comparison of Functional Imaging Modalities
| Feature | FFrCT (via CT CAG) | Stress Testing | Invasive FFR |
| Sensitivity for Ischemia | High | Moderate | High |
| Non-Invasive | Yes | Yes | No |
| Time and Cost Efficiency | Moderate | High | Low |
| Anatomical Assessment | Yes | No | Limited |
FFrCT enhances the role of CT CAG in the diagnostic workflow, especially in intermediate-risk patients, by adding functional relevance to anatomical findings. This integration minimizes unnecessary procedures and refines therapeutic strategies.
CLINICAL APPLICATIONS
CT CAG has established itself as a cornerstone in the diagnostic and management pathways of coronary artery disease (CAD) across various clinical scenarios. Its versatility and accuracy have made it a preferred tool in the following applications:
- Acute Chest Pain Evaluation:
- In the emergency department, CT CAG is used to rule out significant coronary artery disease in low-to-intermediate-risk patients presenting with acute chest pain.
- It aids in early discharge of patients with normal findings, reducing hospitalization costs and duration.
- Stable Chest Pain Assessment:
- For patients with suspected CAD, CT CAG has replaced stress testing in many guidelines as the first-line diagnostic test.
- It provides both anatomical and functional information, helping in risk stratification and decision-making.
- Preoperative Assessment:
- CT CAG is invaluable in preoperative evaluation of patients undergoing non-cardiac surgeries, especially in high-risk populations like those with aortic valve disease or myxomas.
- Monitoring Post-CABG Patients:
- CT CAG is used to assess graft patency and identify issues such as stenosis or occlusion in patients post coronary artery bypass grafting (CABG).
- Complex Coronary Interventions:
- CT CAG provides critical information on coronary anatomy, such as plaque composition, tortuosity, and side-branch involvement, guiding interventional planning.
Table 6: Summary of CT CAG Applications in Clinical Practice
| Clinical Scenario | Role of CT CAG |
| Acute chest pain | Rule out significant CAD, triage for invasive testing |
| Stable chest pain | First-line test for anatomical and functional assessment |
| Preoperative evaluation | Assess coronary arteries in patients undergoing high-risk surgeries |
| Post-CABG monitoring | Evaluate graft patency and detect complications |
| Complex PCI planning | Guide stent selection, plaque modification strategies |
CT CAG has become an indispensable tool in modern cardiology, offering a comprehensive, non-invasive alternative to traditional diagnostic methods, enhancing patient outcomes, and optimizing resource utilization.
EMERGING APPLICATIONS
The field of CT coronary angiography (CT CAG) continues to evolve, with emerging technologies and applications enhancing its diagnostic and prognostic capabilities. Some of the notable advancements include:
- Artificial Intelligence (AI) Integration:
- AI algorithms are now being used to improve image quality, automate plaque analysis, and provide risk stratification for patients.
- AI-driven tools enable precise quantification of plaque burden, identifying high-risk features such as positive remodeling and low-attenuation plaques.
- Peri-Coronary Inflammation Imaging:
- CT imaging techniques are being developed to detect peri-coronary fat attenuation, which serves as a marker of inflammation and early atherosclerosis.
- This provides additional prognostic value for cardiovascular risk assessment.
- Plaque Composition Analysis:
- Advances in software now allow detailed characterization of plaque types (e.g., fibrotic, lipid-rich, calcified) and high-risk features like napkin-ring sign and spotty calcification.
- These insights guide preventive and therapeutic strategies.
- Fractional Flow Reserve CT (FFrCT):
- This technology integrates functional assessment with CT CAG, enabling evaluation of the hemodynamic significance of stenoses without invasive procedures.
- Serial Imaging for Risk Monitoring:
- CT CAG is increasingly used in follow-up studies to monitor disease progression or regression in response to therapy.
- Advanced 3D Imaging:
- 3D reconstructions and virtual reality tools enhance the visualization of coronary anatomy, aiding in pre-procedural planning for interventions.
Table 7: Emerging Applications and Their Clinical Impact
| Emerging Application | Clinical Benefit |
| AI in image interpretation | Improved diagnostic accuracy, faster reporting |
| Peri-coronary inflammation imaging | Early detection of vulnerable plaques and risk stratification |
| Plaque composition analysis | Tailored preventive and therapeutic strategies |
| FFrCT | Non-invasive assessment of functional stenosis significance |
| Serial imaging | Monitoring therapy response and disease progression |
| 3D imaging and virtual reality | Enhanced pre-procedural planning for complex interventions |
PRE-REQUISITE
Table 8: Pre-Requisites for CT CAG
| Category | Requirement | Rationale |
| Patient Preparation | – Fasting for 4–6 hours prior to the procedure. | Reduces artifacts from bowel movements and ensures better image quality. |
| – Heart rate control (< 60 bpm, ideally with beta-blockers). | Minimizes motion artifacts for improved coronary visualization. | |
| – Avoidance of caffeine and smoking on the day of the procedure. | Prevents tachycardia and reduces image degradation. | |
| Renal Function Assessment | – Serum creatinine and eGFR within acceptable ranges (eGFR > 30 mL/min/1.73 m²). | Reduces the risk of contrast-induced nephropathy. |
| – Hydration before and after the scan. | Minimizes renal stress due to contrast media. | |
| Allergy History | – Assessment for prior reactions to iodinated contrast agents. | Avoids allergic reactions; premedication with steroids and antihistamines if necessary. |
| Medication Management | – Discontinuation of metformin 48 hours prior in patients with impaired renal function. | Prevents lactic acidosis in the setting of potential contrast-induced nephropathy. |
| – Temporary adjustment of anticoagulants if required. | Minimizes bleeding risks during invasive procedures post CT CAG, if indicated. | |
| Radiation Consideration | – Avoidance in pregnant women unless absolutely necessary. | Reduces radiation exposure to the fetus. |
| Heart Rate Optimization | – Administration of beta-blockers (e.g., metoprolol) and/or ivabradine if required. | Achieves target heart rate for optimal imaging. |
| Breath-Hold Ability | – Patient must be able to hold breath for 10–15 seconds. | Prevents respiratory motion artifacts. |
| Body Habitus | – Patients with BMI > 35 may require high-performance scanners or alternative imaging methods. | Reduces suboptimal imaging due to excess body mass. |
| Contrast Usage | – Adequate venous access for contrast injection (usually 18–20 gauge cannula). | Ensures proper delivery of contrast media for arterial visualization. |
| ECG Synchronization | – Functional electrocardiogram (ECG) monitoring during the scan. | Allows for proper gating and image acquisition during diastole. |
COMPLICATIONS OF CT-CAG
Table 9: Complications of CT CAG
| Category | Details | Notes |
| Complications | ||
| Contrast-Induced Nephropathy | Acute kidney injury due to iodinated contrast media. | Risk increases in patients with pre-existing renal dysfunction (eGFR < 30 mL/min/1.73 m²). |
| Allergic Reactions | Allergic or hypersensitivity reactions to contrast agents. | Includes rash, itching, anaphylaxis (rare). Premedication can reduce risk. |
| Radiation Exposure | Low to moderate radiation exposure depending on scanner type and protocols used. | Increased risk in younger patients or those requiring repeated imaging. |
| Cardiac Arrhythmias | Bradycardia or transient arrhythmias during beta-blocker administration. | Monitor heart rhythm during preparation. |
| Adverse Effects of Medications | Side effects of beta-blockers (e.g., hypotension, bronchospasm) or nitroglycerin (e.g., headache). | Requires careful patient selection and monitoring. |
| Misinterpretation Risks | Artifacts from motion, calcification, or poor contrast timing can lead to misdiagnosis. | May necessitate further invasive testing (e.g., ICA). |
Table 10: Contraindications of CT-CAG
| Contraindications | Details | Notes |
| Severe Renal Dysfunction | eGFR < 30 mL/min/1.73 m² or acute kidney injury. | Avoid contrast media unless absolutely necessary and pre-treat appropriately. |
| Contrast Media Allergy | History of severe allergic reactions to iodinated contrast. | Consider non-contrast imaging or use alternative modalities. |
| Pregnancy | Avoid unless the benefits outweigh the risks. | Risk of fetal radiation exposure; non-ionizing imaging preferred. |
| Inability to Control Heart Rate | Patients with arrhythmias (e.g., atrial fibrillation) or contraindications to beta-blockers. | Results in suboptimal image quality due to motion artifacts. |
| Severe Claustrophobia | Patients unable to tolerate confined spaces for CT scan. | Sedation may be required but increases procedural risk. |
| Morbid Obesity | Patients exceeding the scanner’s weight limit (varies by model). | May need alternative imaging strategies. |
| Active Infection or Unstable ACS | Hemodynamic instability or sepsis. | Prioritize stabilization over non-urgent imaging. |
LIMITATIONS OF CT CAG
CT Coronary Angiography (CT CAG) offers significant diagnostic advantages, but it has some limitations that must be considered when deciding its role in patient management.
| Limitation | Details | Impact |
| Radiation Exposure | Despite advancements, radiation exposure remains a concern, particularly in younger patients or those requiring repeat scans. | Long-term cancer risks, especially in cumulative exposure scenarios. |
| Contrast-Induced Nephropathy | Requires iodinated contrast agents, posing risks for patients with impaired renal function. | Limits its use in patients with severe renal dysfunction or in dehydration states. |
| Limited Functional Assessment | CT CAG primarily assesses anatomical features; functional data (e.g., ischemia) requires integration with FFrCT or other tests. | May necessitate additional tests to evaluate physiological significance of stenosis. |
| Image Quality Issues | Image quality may be degraded in patients with high heart rates, arrhythmias, obesity, or heavy coronary calcification. | Can lead to nondiagnostic scans or false-positive/negative results. |
| Artifacts | Motion artifacts, beam-hardening from calcifications, or misalignment during ECG gating can impair accuracy. | Potential for misinterpretation and need for repeat or alternative testing. |
| Cost and Accessibility | Higher upfront costs and limited availability in some healthcare settings. | Limits widespread use, particularly in resource-limited environments. |
| Overdiagnosis and Overtreatment | Identification of non-obstructive plaques can lead to unnecessary interventions or follow-ups. | May increase healthcare costs and patient anxiety without clear clinical benefit. |
| Limited Applicability in Acute Settings | In patients with hemodynamic instability or acute myocardial infarction, CT CAG may delay definitive invasive testing. | Unsuitable for critical or unstable patients requiring immediate intervention. |
| Weight and Size Constraints | Most CT scanners have weight and size limits, making imaging difficult for morbidly obese patients. | Reduces accessibility for patients with high BMI. |
| Radiation-Sensitive Populations | Not suitable for pregnant women due to potential fetal exposure. | Necessitates the use of alternative imaging modalities like MRI or echocardiography. |
TRIALS ON CT CAG VS INVASIVE CAG
Table 12 : Key Trials Comparing CT CAG vs. Invasive CAG
| Trial | Year | Study Population | Key Findings | Clinical Implications |
| SCOT-HEART | 2015 | 4,146 patients with stable chest pain | CT CAG improved diagnosis of CAD, reduced rates of MI and CAD-related death by 41% over 5 years. | Demonstrated the prognostic and diagnostic superiority of CT CAG, supporting its use in stable CAD. |
| PROMISE | 2015 | 10,003 symptomatic patients | CT CAG had similar outcomes to functional testing but identified more atherosclerosis. | Highlighted CT CAG’s value in assessing CAD burden and guiding preventive therapies. |
| DISCOVER-FLOW | 2011 | 103 patients with intermediate lesions | CT-derived FFR (FFrCT) was highly accurate compared to invasive FFR for functional stenosis assessment. | Showed potential of CT CAG with FFrCT to reduce unnecessary ICAs. |
| PLATFORM | 2016 | 584 patients with intermediate risk | FFrCT-based strategy reduced unnecessary invasive angiographies by 61%. | Reinforced the functional utility of FFrCT alongside CT CAG for decision-making. |
| CRESCENT | 2016 | 350 patients with stable angina | CT CAG was faster and safer than invasive coronary angiography for initial CAD evaluation. | Advocated for CT CAG as a frontline test in low-to-intermediate risk patients. |
| ISCHEMIA | 2019 | 5,179 patients with moderate ischemia | CT CAG excluded left main disease in 11% of patients, proving a reliable gatekeeper for ICA. | Supported the use of CT CAG in stable ischemic heart disease, reducing unnecessary invasive tests. |
| VERDICT | 2021 | Non-ST elevation ACS patients | Early CT CAG accurately identified significant CAD; comparable to invasive angiography within 2.5 hours. | Demonstrated CT CAG’s utility in rapid triage for ACS patients. |
| CONFIRM | 2012 | 27,125 patients | CT CAG-derived plaque burden correlated strongly with major adverse cardiovascular events (MACE). | Highlighted the prognostic importance of CT CAG-derived data in CAD risk stratification. |
BIBILOGRAPHY
- Widmer RJ, Rosol ZP, Banerjee S, Sandoval Y, Schussler JM. Cardiac computed tomography angiography in the evaluation of coronary artery disease: An interventional perspective. J Soc Cardiovasc Angiogr Interv. 2024;3:101301. doi:10.1016/j.jscai.2024.101301.
- Budoff MJ, Lakshmanan S, Toth PP, Hecht HS, Shaw LJ, Maron DJ, et al. Cardiac CT angiography in current practice: An American Society for Preventive Cardiology clinical practice statement. Am J Prev Cardiol. 2022;9:100318. doi:10.1016/j.ajpc.2022.100318.
- SCOT-HEART investigators. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): An open-label, parallel-group, multicentre trial. Lancet. 2015;385(9985):2383-91. doi:10.1016/S0140-6736(15)60291-4.
- Douglas PS, Hoffmann U, Patel MR, Mark DB, Al-Khalidi HR, Cavanaugh B, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 2015;372(14):1291-300. doi:10.1056/NEJMoa1415516.
- Nørgaard BL, Leipsic J, Gaur S, Seneviratne S, Ko BS, Ito H, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: The NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol. 2014;63(12):1145-55. doi:10.1016/j.jacc.2013.11.043.
- Curzen N, Nolan J, Zaman A, Nørgaard BL, Redwood S. Does the routine availability of CT-derived fractional flow reserve influence management of patients with stable chest pain compared to CT angiography alone? The PLATFORM study. J Am Coll Cardiol. 2016;68(5):435-45. doi:10.1016/j.jacc.2016.05.057.
- Newby DE, Adamson PD, Berry C, Boon NA, Dweck MR, Flather MD, et al. Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med. 2018;379(10):924-33. doi:10.1056/NEJMoa1805971.
- Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O’Brien SM, Boden WE, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382(15):1395-407. doi:10.1056/NEJMoa1915922.
- Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40(3):237-69. doi:10.1093/eurheartj/ehy462.
- Pontone G, Andreini D, Guaricci AI, Guglielmo M, Baggiano A, Mushtaq S, et al. Prognostic utility of coronary CT angiography and stress imaging: Insights from the EVINCI study (Evaluation of Integrated Cardiac Imaging for the Detection and Characterization of Ischemic Heart Disease). J Am Coll Cardiol. 2015;66(13):1605-15. doi:10.1016/j.jacc.2015.07.070.
About the Author
Dr. Akif Ahamad Baig is a distinguished cardiologist and medical educator based in India. He holds an MBBS degree, a DNB in General Medicine, and a DM in Cardiology. Dr. Baig is the CEO, Founder, and Content Head of InfusionMedz.com, a platform dedicated to medical education, teleconsultation services, and health awareness.