DRUGS FOR DYSLIPIDEMIA
Lipid Metabolism
1. Digestion and Absorption
- Dietary fats (mainly triglycerides) are
broken down by pancreatic lipase into free fatty acids and monoglycerides in
the small intestine. - Bile salts emulsify fats, aiding their digestion
and absorption by forming micelles. - Free fatty acids and monoglycerides are absorbed by
intestinal cells (enterocytes), where they are re-esterified into
triglycerides.
2. Lipid Transport
- Chylomicrons: In enterocytes, triglycerides
are packaged with cholesterol and proteins to form chylomicrons, which are
transported via the lymphatic system into the bloodstream. - VLDL (Very Low-Density Lipoproteins): In the
liver, triglycerides and cholesterol are packaged into VLDL particles,
which deliver triglycerides to tissues.
3. Lipid Utilization
- Lipolysis: In tissues, lipoprotein lipase
breaks down triglycerides in chylomicrons and VLDL into free fatty acids
and glycerol, which are taken up by cells for energy (via β-oxidation) or
storage in adipose tissue. - β-Oxidation: In mitochondria, fatty acids
are oxidized to produce acetyl-CoA, which enters the Krebs
cycle for energy production, generating ATP. - Ketogenesis: In cases of excess acetyl-CoA
(e.g., fasting), it is converted into ketone bodies in
the liver, used as an alternative energy source.
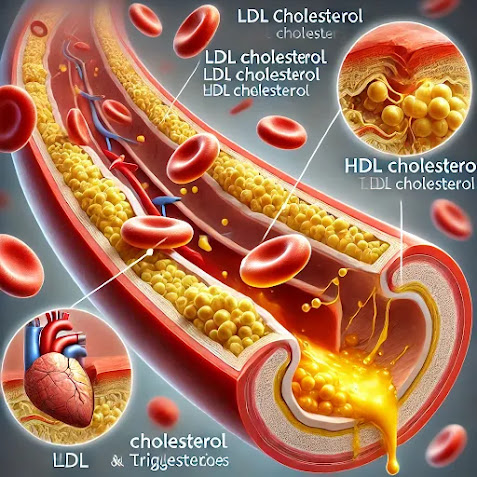
4. Cholesterol Metabolism
- Synthesis: The liver synthesizes cholesterol
de novo from acetyl-CoA via the HMG-CoA reductase pathway. - Excretion: Excess cholesterol is converted
into bile acids and excreted in bile. - LDL-C and HDL-C: LDL delivers cholesterol to
peripheral tissues, while HDL (produced in the liver and intestines)
retrieves excess cholesterol from tissues and returns it to the liver for
excretion (reverse cholesterol transport).
5. Fat Storage
- Excess dietary fat is stored as triglycerides in
adipose tissue. - During fasting or energy needs, stored
triglycerides are broken down (lipolysis) into free fatty acids and
glycerol, which are released into the bloodstream for energy production.
Classification of drugs used for dyslipidemia:
1. HMG-CoA Reductase
Inhibitors (Statins)
- Examples: Atorvastatin, Simvastatin,
Rosuvastatin
2. Bile Acid Sequestrants
- Examples: Cholestyramine, Colesevelam,
Colestipol
3. Fibrates (Fibric Acid
Derivatives)
- Examples: Fenofibrate, Gemfibrozil
4. Nicotinic Acid (Niacin)
- Examples: Niacin (Vitamin B3)
5. Cholesterol Absorption
Inhibitors
- Example: Ezetimibe
- Mechanism of Action: Inhibits the
absorption of cholesterol in the small intestine, leading to reduced
6. Omega-3 Fatty Acids
- Examples: Eicosapentaenoic acid (EPA),
Docosahexaenoic acid (DHA)
7. PCSK9 Inhibitors
- Examples: Alirocumab, Evolocumab
8. Selective Peroxisome
Proliferator-Activated Receptor-Delta (PPAR-δ) Agonists
- Examples: Tesaglitazar
9. Bempedoic Acid
- Mechanism of Action: Inhibits ATP
citrate lyase (ACL), an enzyme involved in cholesterol synthesis, reducing
LDL-C levels.
10. CETP Inhibitors
(Cholesteryl Ester Transfer Protein Inhibitors)
- Examples: Anacetrapib, Dalcetrapib
(investigational drugs)
Statins
Statins, also known as HMG-CoA
reductase inhibitors, are the most commonly prescribed class of drugs for
the treatment of dyslipidemia, primarily targeting elevated LDL-C (Low-Density
Lipoprotein Cholesterol). They have been extensively studied and proven to
reduce cardiovascular events, morbidity, and mortality in both primary and
secondary prevention of cardiovascular diseases.
Mechanism of Action
- Statins inhibit HMG-CoA reductase, the
enzyme responsible for the conversion of HMG-CoA to mevalonate, a key
precursor in the biosynthesis of cholesterol. - By inhibiting this rate-limiting step in
cholesterol synthesis, statins lead to a decrease in intracellular
cholesterol levels in the liver. - The liver responds by upregulating LDL receptors on
the hepatocyte surface, which increases the clearance of circulating LDL-C
from the blood.
Pharmacokinetics
- Absorption: Statins are absorbed
variably after oral administration. The bioavailability of statins is
generally low due to extensive first-pass hepatic metabolism. - Metabolism: Most statins are
metabolized in the liver by the cytochrome P450 (CYP) enzyme system. For
example: - Atorvastatin and Simvastatin are metabolized
by CYP3A4. - Rosuvastatin and Pravastatin are less dependent on
CYP enzymes. - Excretion: Statins and their
metabolites are mainly excreted via the liver (bile) and to a lesser
extent via the kidneys.
Half-lives of common statins:
- Atorvastatin: 14 hours
- Rosuvastatin: 19 hours
- Simvastatin: 2 hours
- Pravastatin: 1.5-2 hours
Pharmacodynamics
- LDL-C Reduction: Statins significantly
reduce LDL-C levels (by 20–60%), depending on the dose and potency. - Triglyceride Reduction: Statins also
reduce triglyceride levels by 10–30%. - HDL-C Increase: Statins modestly
increase HDL-C levels by 5–10%. - Pleiotropic Effects: In addition to
their lipid-lowering action, statins exert several “pleiotropic”
effects, including: - Improving endothelial function
- Stabilizing atherosclerotic plaques
- Reducing vascular inflammation
- Decreasing oxidative stress
Indications
- Primary prevention of cardiovascular
events in patients with elevated LDL-C levels. - Secondary prevention in patients with
established cardiovascular disease (e.g., post-myocardial infarction,
stroke). - Management of dyslipidemia, particularly in
patients with high LDL-C or mixed dyslipidemia. - Familial hypercholesterolemia, both
heterozygous and homozygous, as adjunctive therapy.
Adverse Effects
- Myopathy and Rhabdomyolysis: Statins
can cause muscle-related side effects, ranging from mild myalgia to severe
rhabdomyolysis. Risk is dose-dependent and higher with concurrent use of
drugs that inhibit CYP3A4. - Hepatotoxicity: Statins can cause mild
elevations in liver transaminases. Severe liver injury is rare, but liver
function tests are recommended at baseline and during treatment if
clinically indicated. - New-Onset Diabetes: Statin therapy has
been associated with a small increased risk of developing type 2 diabetes,
particularly at high doses. - Cognitive Effects: Rarely, statins have
been associated with reversible cognitive effects such as memory loss and
confusion.
Contraindications
- Active liver disease or unexplained persistent
elevations in liver enzymes. - Pregnancy and breastfeeding, as statins can cause
teratogenic effects. - Hypersensitivity to any component of the statin
formulation.
Drug Interactions
- CYP3A4 Inhibitors: Drugs such as azole
antifungals (e.g., ketoconazole), macrolide antibiotics (e.g.,
erythromycin), protease inhibitors (e.g., ritonavir), and grapefruit juice
can increase statin levels and the risk of myopathy. - Fibrates: Concomitant use of fibrates,
especially gemfibrozil, increases the risk of myopathy and rhabdomyolysis. - Warfarin: Statins may potentiate the
effect of warfarin, increasing the risk of bleeding.
Examples of Statins (Potency and
Dosing)
- Atorvastatin : Moderate-High potency,
10–80 mg/day - Rosuvastatin : High potency, 5–40
mg/day - Simvastatin : Moderate potency, 10–40
mg/day - Pravastatin : Low-Moderate potency,
10–80 mg/day - Lovastatin : Low potency, 20–80 mg/day
- Fluvastatin : Low potency, 20–80 mg/day
Clinical Considerations
- Dosing: Statins are generally
administered once daily, with atorvastatin and rosuvastatin having long
half-lives that allow for flexibility in dosing time. Simvastatin and
lovastatin should be taken in the evening for maximum efficacy, as
cholesterol synthesis is highest at night. - Monitoring: Liver function tests and CK
(creatine kinase) levels should be monitored in patients at risk of
adverse effects, especially those on high doses or with concomitant drug
interactions.
Fibrates
Fibrates, also known as fibric
acid derivatives, are a class of lipid-lowering drugs primarily used to
reduce triglyceride levels and, to a lesser extent, to increase HDL-C
(High-Density Lipoprotein Cholesterol). Fibrates are particularly effective in
patients with hypertriglyceridemia and mixed dyslipidemia.
Mechanism of Action
- Fibrates activate the peroxisome
proliferator-activated receptor-alpha (PPAR-α), a nuclear
transcription factor. - Activation of PPAR-α leads to the following
metabolic effects: - Increased lipoprotein lipase (LPL) activity:
This enhances the hydrolysis of triglycerides in VLDL (Very Low-Density
Lipoprotein) and chylomicrons, reducing plasma triglyceride levels. - Decreased production of apoC-III: ApoC-III
inhibits lipoprotein lipase; thus, its suppression further enhances
triglyceride breakdown. - Increased fatty acid oxidation: In the
liver and muscles, this process reduces the availability of fatty acids
for triglyceride synthesis. - Increased HDL-C: Fibrates increase the
synthesis of apolipoproteins A-I and A-II, which leads to enhanced
production of HDL particles.
Pharmacokinetics
- Absorption: Fibrates are well-absorbed
when taken orally, especially when consumed with food, which enhances
their bioavailability. - Metabolism: Fibrates are metabolized in
the liver through glucuronidation and are not significantly metabolized by
the cytochrome P450 enzyme system. - Excretion: Primarily excreted via the
kidneys as glucuronide conjugates. Dosage adjustments are required in
patients with renal impairment.
Pharmacodynamics
- Reduction in Triglycerides: Fibrates
are particularly effective in reducing plasma triglyceride levels (by
30–50%). - Increase in HDL-C: They increase HDL-C
levels by 10–20%. - Effect on LDL-C: The effect of fibrates
on LDL-C is variable. In patients with hypertriglyceridemia, fibrates may
lower LDL-C by 5–20%, but in some cases, they can increase LDL-C levels,
especially in patients with very high triglycerides.
Indications
- Hypertriglyceridemia: Fibrates are the
first-line agents for the treatment of severe hypertriglyceridemia,
especially when the risk of pancreatitis is high. - Mixed dyslipidemia: In patients with
elevated triglycerides and low HDL-C, fibrates are used in combination
with statins. - Dysbetalipoproteinemia (Type III
hyperlipoproteinemia): Fibrates are particularly effective in this
rare genetic disorder characterized by increased triglycerides and
cholesterol.
Adverse Effects
- Myopathy and Rhabdomyolysis: Fibrates can
cause muscle-related side effects, such as myopathy, especially when used
in combination with statins. The risk of rhabdomyolysis is higher with
gemfibrozil compared to fenofibrate. - Gastrointestinal Disturbances: Fibrates may
cause nausea, abdominal pain, and dyspepsia. - Cholelithiasis (Gallstones): Fibrates
increase the cholesterol content of bile, predisposing to gallstone
formation. - Hepatotoxicity: Fibrates may cause mild
elevations in liver enzymes. Severe liver toxicity is rare but can occur. - Renal Impairment: Fibrates can increase
serum creatinine levels and should be used cautiously in patients with
pre-existing renal impairment.
Contraindications
- Severe renal impairment: Fibrates are
excreted by the kidneys, and their use is contraindicated in patients with
significant renal dysfunction (e.g., GFR < 30 mL/min). - Liver disease: Fibrates should not be used
in patients with active liver disease, including cirrhosis or hepatitis. - Gallbladder disease: Due to the risk of
gallstones, fibrates are contraindicated in patients with pre-existing
gallbladder disease. - Hypersensitivity: Patients with a known
hypersensitivity to fibrates should avoid them.
Examples of Fibrates
- Fenofibrate
- Dose: 54–160 mg once daily.
- Metabolism: Fenofibrate is a prodrug that
is converted to its active metabolite fenofibric acid. - Excretion: Primarily excreted in the urine.
- Gemfibrozil
- Dose: 600 mg twice daily.
- Metabolism: Gemfibrozil undergoes extensive
hepatic glucuronidation. - Excretion: Mainly excreted in the urine.
- Drug Interactions: Higher risk of myopathy
when combined with statins compared to fenofibrate.
Bile Acid Sequestrants
1. Mechanism of Action:
- Bile acid sequestrants (resins) bind bile acids in
the intestine, preventing their reabsorption. - This forces the liver to use more cholesterol to
synthesize new bile acids, thereby reducing the cholesterol pool and
increasing LDL receptor activity, which lowers circulating LDL-C.
2. Examples:
- Cholestyramine
- Colestipol
- Colesevelam
3. Effects:
- Decreases LDL-C by 15-30%.
- Slight increase in HDL-C.
- May increase triglycerides (especially
in patients with hypertriglyceridemia).
4. Adverse Effects:
- Gastrointestinal issues: Constipation,
bloating, abdominal discomfort. - May interfere with the absorption of fat-soluble
vitamins (A, D, E, K) and other medications (e.g., warfarin, digoxin).
5. Indications:
- Primarily used to lower LDL-C in patients with
hypercholesterolemia. - Can be combined with statins for additive effects.
6. Contraindications:
- Complete biliary obstruction.
- Severe hypertriglyceridemia (due to
risk of increasing triglycerides).
Cholesterol Absorption Inhibitors
1. Mechanism of Action:
- The primary cholesterol absorption inhibitor, Ezetimibe,
works by inhibiting the Niemann-Pick C1-Like 1 (NPC1L1) protein
in the small intestine. - This prevents the absorption of dietary and biliary
cholesterol, reducing the cholesterol delivered to the liver and prompting
the liver to take up more LDL-C from the bloodstream.
2. Example:
- Ezetimibe (Zetia)
3. Effects:
- Decreases LDL-C by 15-20%.
- Minimal effect on HDL-C and triglycerides.
- Often combined with statins for synergistic LDL-C
reduction.
4. Adverse Effects:
- Generally well-tolerated.
- Mild gastrointestinal symptoms (e.g., diarrhea,
abdominal pain). - Rarely, elevated liver enzymes when used in
combination with statins.
5. Indications:
- Used to reduce LDL-C in patients with hypercholesterolemia.
- Often prescribed as an add-on therapy
to statins when additional LDL-C lowering is needed.
6. Contraindications:
- Severe hepatic impairment.
- Hypersensitivity to the drug or any of
its components.
PCSK9 Inhibitors
Mechanism of Action:
- PCSK9 inhibitors are monoclonal antibodies that
target proprotein convertase subtilisin/kexin type 9 (PCSK9). - PCSK9 normally binds to LDL receptors on liver
cells, promoting their degradation. - By inhibiting PCSK9, these drugs increase the
number of LDL receptors available to clear LDL-C from the
bloodstream, thereby reducing LDL-C levels.
Examples:
- Alirocumab
- Evolocumab
Effects:
- Significant reduction in LDL-C by
50-60%. - Moderate reduction in triglycerides and increase in
HDL-C. - Additive effect when combined with statins or other
lipid-lowering agents.
Adverse Effects:
- Injection site reactions (as they are
given subcutaneously). - Flu-like symptoms, such as upper respiratory tract
infections. - Rare reports of cognitive effects, such as
confusion or memory issues.
Indications:
- Familial hypercholesterolemia (heterozygous
or homozygous). - Atherosclerotic cardiovascular disease patients
who require additional LDL-C lowering despite statin therapy. - Patients intolerant to statins.
Contraindications:
- Hypersensitivity to the drug or its
components. - Pregnancy and breastfeeding (use with
caution, as the effects have not been well-studied).
Administration:
- Given by subcutaneous injection every
2–4 weeks, depending on the drug and dosage.
Nicotinic Acid (Niacin)
- Mechanism: Reduces VLDL and LDL
synthesis in the liver, while increasing HDL-C. - Effects: Lowers LDL-C and
triglycerides, significantly increases HDL-C. - Adverse Effects: Flushing,
hyperglycemia, hyperuricemia (gout), hepatotoxicity.
Omega-3 Fatty Acids
- Examples: Eicosapentaenoic acid (EPA),
Docosahexaenoic acid (DHA) - Mechanism: Reduce hepatic triglyceride
synthesis. - Effects: Primarily reduce
triglycerides, with minimal effects on LDL-C and HDL-C. - Adverse Effects: GI discomfort, fishy
aftertaste, increased risk of bleeding.
4. Bempedoic Acid
- Mechanism: Inhibits ATP citrate lyase
(ACL), an enzyme involved in cholesterol biosynthesis. - Effects: Lowers LDL-C by 15-20%.
- Adverse Effects: Muscle pain, elevated
uric acid levels, potential increase in liver enzymes.
Newer Drugs for Dyslipidemia
1. Inclisiran
- Mechanism: Small interfering RNA
(siRNA) that targets PCSK9 mRNA, reducing PCSK9 synthesis in the liver. - Effect: Significantly reduces LDL-C (up
to 50%) by increasing LDL receptor availability. - Administration: Subcutaneous injection
every 6 months. - Adverse Effects: Injection site
reactions, nasopharyngitis.
2. Bempedoic Acid
- Mechanism: Inhibits ATP citrate lyase
(ACL), an enzyme upstream of HMG-CoA reductase in the cholesterol
biosynthesis pathway. - Effect: Lowers LDL-C by 15–20%, often
used as an adjunct to statins. - Adverse Effects: Increased uric acid
(risk of gout), muscle pain, elevated liver enzymes.
3. Evinacumab
- Mechanism: Monoclonal antibody against
angiopoietin-like 3 (ANGPTL3), a regulator of lipid metabolism. - Effect: Reduces LDL-C, triglycerides,
and HDL-C, particularly effective in patients with homozygous familial
hypercholesterolemia. - Administration: Intravenous infusion
every 4 weeks. - Adverse Effects: Flu-like symptoms, GI
discomfort.
4. Lomitapide
- Mechanism: Inhibits microsomal
triglyceride transfer protein (MTP), reducing VLDL and LDL particle
formation. - Effect: Dramatic reduction in LDL-C
(40-50%), primarily used in patients with homozygous familial
hypercholesterolemia. - Adverse Effects: GI disturbances, liver
enzyme elevation, hepatotoxicity.
5. Mipomersen
- Mechanism: Antisense oligonucleotide
targeting apolipoprotein B (apoB) mRNA, reducing LDL-C synthesis. - Effect: Lowers LDL-C (up to 25%), used
for homozygous familial hypercholesterolemia. - Adverse Effects: Injection site
reactions, flu-like symptoms, liver toxicity.
6. ANGPTL3 Inhibitors
- Examples: Evinacumab, investigational
drugs targeting ANGPTL3. - Mechanism: Inhibit angiopoietin-like 3
(ANGPTL3), which regulates lipid metabolism, leading to reductions in
LDL-C, triglycerides, and HDL-C. - Effect: Significant reductions in LDL-C
and triglycerides, especially in patients with genetic lipid disorders.