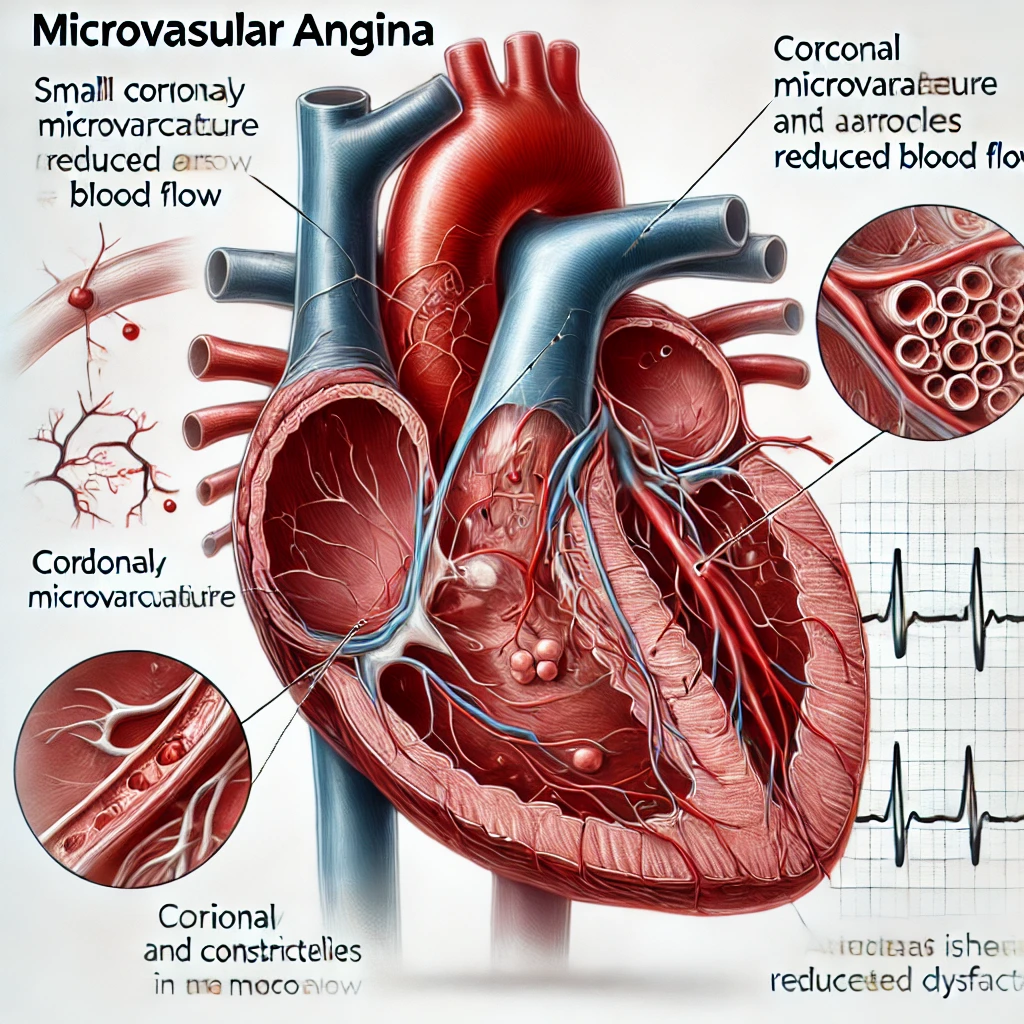
Microvascular angina (MVA), also known as cardiac syndrome X or ischemia with no obstructive coronary arteries (INOCA), is characterized by angina-like chest pain, myocardial ischemia, and non-obstructive coronary arteries on angiography. This condition primarily affects the microvasculature, particularly the small coronary arterioles (≤200 μm in diameter), leading to impaired myocardial perfusion and recurrent ischemic symptoms without significant stenosis in the larger coronary arteries. MVA is increasingly recognized in cardiology for its impact on patients’ quality of life and potential for adverse cardiovascular outcomes.
Pathophysiology of Microvascular Angina
The pathophysiology of MVA is multifactorial, involving a combination of endothelial dysfunction, smooth muscle hyperreactivity, and impaired coronary flow reserve (CFR). Key mechanisms include:
- Endothelial Dysfunction: The endothelium’s impaired ability to release vasodilators (e.g., nitric oxide) leads to diminished vasodilation and increased vasoconstriction in coronary microvessels, reducing myocardial blood flow.
- Microvascular Spasm and Smooth Muscle Hyperreactivity: Hyperreactivity of the vascular smooth muscle, triggered by various stimuli, can lead to coronary microvascular spasm. Unlike the larger epicardial coronary arteries, microvasculature has a more significant influence from factors like metabolic demands and neural inputs.
- Reduced Coronary Flow Reserve (CFR): CFR, the ratio of maximal coronary blood flow during stress to basal flow, is often reduced in MVA. This indicates an inability of coronary microvessels to increase perfusion adequately in response to increased myocardial demand.
- Impaired Autoregulation and Structural Changes: Abnormal microvascular remodeling, including changes in microvascular density or vessel lumen diameter, may contribute to impaired blood flow.
Inflammation and oxidative stress may also contribute to endothelial dysfunction and microvascular spasm, exacerbating ischemia.
Clinical Presentation
Patients with MVA typically present with angina-like chest pain, often exertional or occurring at rest, which is similar to the presentation of obstructive coronary artery disease (CAD). However, MVA is often associated with prolonged episodes, pain unresponsive to nitrates, and symptoms that may not correlate directly with exertion levels.
Additional symptoms may include:
- Dyspnea: Shortness of breath is frequently reported.
- Fatigue: A notable feature that can impair daily functioning.
- Reduced Exercise Tolerance: Due to ischemic symptoms during physical activity.
Diagnostic Evaluation
- Coronary Angiography: The gold standard for ruling out obstructive CAD, coronary angiography in MVA patients typically shows non-obstructive coronary arteries (<50% stenosis).
- Coronary Function Testing: This includes acetylcholine or adenosine challenge testing to assess endothelial function and vasomotor reactivity. Impaired vasodilation or microvascular spasm on testing supports an MVA diagnosis.
- Assessment of Coronary Flow Reserve (CFR): Non-invasive techniques, such as positron emission tomography (PET), cardiac magnetic resonance imaging (CMRI), and transthoracic Doppler echocardiography, are used to measure CFR, with values <2.5 suggestive of MVA.
- Cardiac Stress Testing: Exercise or pharmacological stress testing may reveal ischemia, although traditional ECG stress tests may not always show changes due to the microvascular nature of the ischemia.
- Microvascular Imaging: Techniques like CMRI and PET imaging can be instrumental in visualizing microvascular dysfunction and evaluating myocardial blood flow.
Management of Microvascular Angina
Management of MVA is focused on symptom control, improving microvascular function, and reducing cardiovascular risk. Treatment strategies include:
- Antianginal Therapy:
- Beta-blockers: May improve symptoms by reducing myocardial oxygen demand.
- Calcium Channel Blockers (CCBs): Especially non-dihydropyridine CCBs like diltiazem and verapamil, which may alleviate microvascular spasm.
- Nitrates: Though typically less effective in MVA than in obstructive CAD, they may benefit some patients.
- Ranolazine: Effective in reducing anginal episodes by inhibiting late sodium current in myocardial cells.
- Ivabradine: An If channel inhibitor that reduces heart rate without affecting blood pressure, improving symptoms in some MVA patients.
- Vasodilator and Endothelial Function Modulators:
- Angiotensin-Converting Enzyme Inhibitors (ACEIs) or Angiotensin II Receptor Blockers (ARBs): May improve endothelial function and decrease microvascular constriction.
- Statins: Provide pleiotropic benefits, including improving endothelial function and reducing inflammation.
- Lifestyle Modification and Risk Factor Management:
- Aggressive management of cardiovascular risk factors such as hypertension, hyperlipidemia, and diabetes is crucial.
- Exercise Training: Cardiac rehabilitation programs with tailored exercise may improve endothelial function and enhance symptoms.
- Emerging Therapies:
- L-Arginine and L-Citrulline Supplementation: May increase nitric oxide bioavailability and improve microvascular function, although evidence is limited.
- Antioxidants: Some studies suggest that antioxidants may help reduce oxidative stress and improve symptoms in MVA.
Prognosis and Outcomes
While traditionally considered a benign condition, recent studies indicate that MVA is associated with an increased risk of adverse cardiovascular events, including myocardial infarction, heart failure, and reduced quality of life. Risk stratification is essential, especially as some patients may have high-risk features, including severe endothelial dysfunction or markedly reduced CFR. Long-term management focusing on lifestyle modifications, symptom relief, and monitoring of cardiovascular health is crucial for improving prognosis and quality of life in MVA patients.
Conclusion
Microvascular angina is a complex condition resulting from coronary microvascular dysfunction, presenting with angina-like symptoms and associated with considerable morbidity. Effective management includes a combination of antianginal therapy, risk factor modification, and potentially emerging therapies to improve endothelial function and alleviate symptoms. Ongoing research is vital to better understand its pathophysiology and develop targeted treatments that address the specific mechanisms underlying MVA.