Coronary artery disease remains a leading cause of morbidity and mortality worldwide. While lifestyle modifications, pharmacotherapy, and revascularization have improved outcomes, certain patient groups, including those with refractory angina or CMD, often experience persistent symptoms despite conventional treatments. For these patients, EECP offers a unique, non-invasive alternative. Since its approval by the FDA for refractory angina, EECP has been the subject of numerous studies aimed at elucidating its mechanisms and assessing its clinical efficacy.
2. Mechanisms of EECP
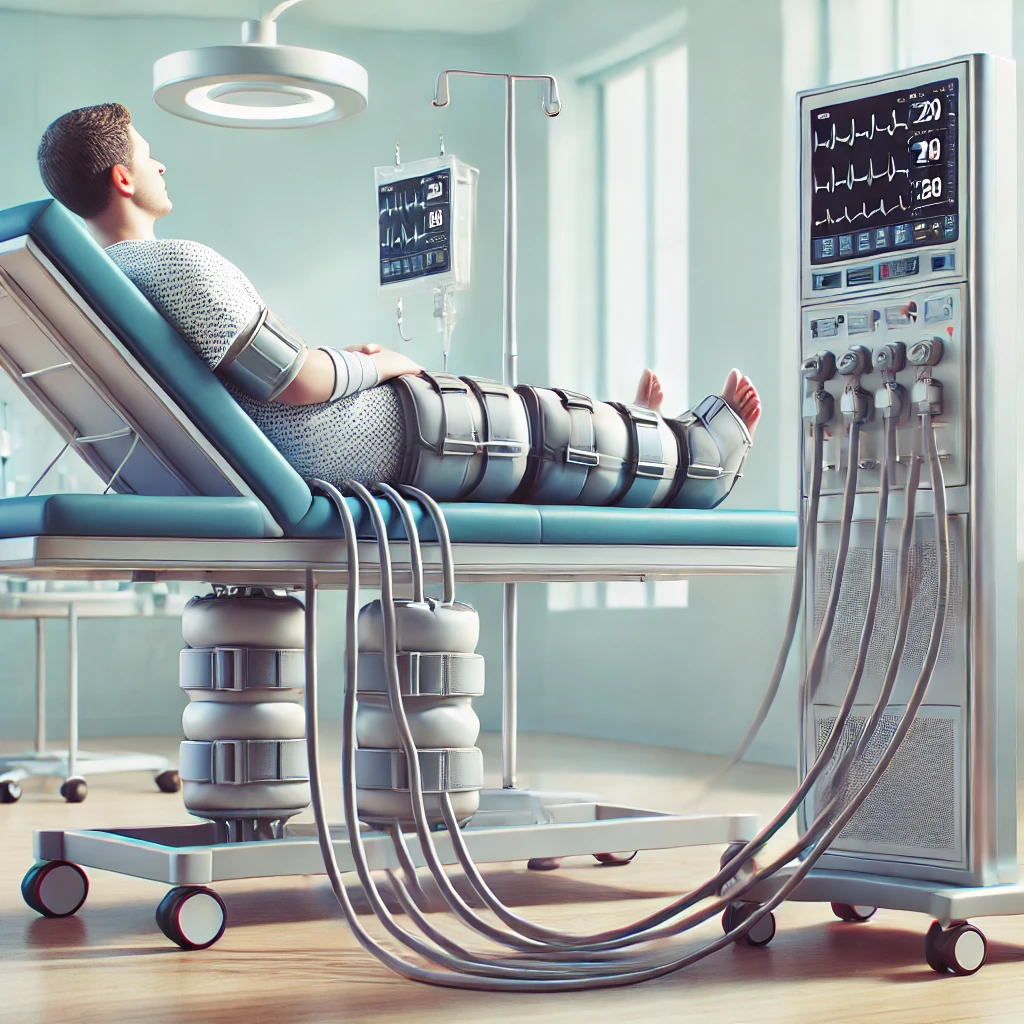
EECP operates through an external, sequential inflation of cuffs on the calves, thighs, and buttocks during the diastolic phase of the cardiac cycle. This results in a retrograde aortic flow, which increases coronary perfusion and enhances myocardial oxygenation during diastole. Key mechanisms include:
- Diastolic Augmentation: By raising diastolic pressure, EECP supports myocardial perfusion, which is particularly beneficial in ischemic regions.
- Collateral Vessel Formation: Studies suggest EECP may promote angiogenesis, enhancing collateral circulation in the coronary arteries.
- Reduction in Left Ventricular Afterload: During deflation, EECP rapidly decreases vascular resistance, which can reduce the workload on the heart and improve overall cardiac function.
- Endothelial Function Improvement: EECP is also associated with improved endothelial function, potentially through upregulation of nitric oxide production, which supports vasodilation and vascular health.
3. Clinical Evidence and Recent Studies (2020 Onward)
Several studies from 2020 onwards have provided updated insights into EECP’s efficacy and safety for CAD and related complications.
- Transfer Function Analysis of Peripheral Signals
A 2024 study by Zhang et al. analyzed changes in peripheral ultrasound signals in CAD patients post-EECP, using transfer function (TF) analysis. This research showed significant changes in peripheral vascular responses, shedding light on EECP’s physiological effects and providing potential markers for treatment efficacy (Zhang et al., 2024, ResearchSquare) - Coronary Microvascular Dysfunction and EECP (EECP-CMD II)
Cao et al. (2024) examined EECP’s role in treating CMD in CAD patients, specifically focusing on coronary microcirculation dysfunction (CMD). This randomized control trial highlighted EECP’s potential in improving microcirculation, especially in cases where pharmacological approaches were insufficient (Cao et al., 2024, BMJ Open). - EECP in Refractory Angina
A 2022 study published in Cardiovascular Revascularization Medicine discussed EECP as a viable alternative for patients with refractory angina who are not candidates for revascularization. EECP was shown to reduce anginal episodes, improve exercise tolerance, and enhance quality of life among these patients.
4. Mechanisms Under Investigation
Recent research has been examining the cellular and molecular pathways influenced by EECP. It is hypothesized that EECP may increase vascular endothelial growth factor (VEGF) expression, promoting angiogenesis. Additionally, EECP may enhance nitric oxide bioavailability, improving endothelial function, which is often compromised in CAD. Advanced imaging techniques, such as functional MRI and positron emission tomography (PET), are now being used to explore these molecular changes in greater detail.
5. Applications in Clinical Practice
EECP is primarily recommended for:
- Refractory Angina: For patients unresponsive to medications and unsuitable for invasive procedures, EECP has demonstrated symptom relief and improved exercise tolerance.
- Coronary Microvascular Dysfunction: CMD, a condition with limited treatment options, shows promising response rates to EECP therapy as evidenced in the EECP-CMD II trial.
- Heart Failure: Although traditionally used in angina management, emerging data suggest EECP could be beneficial for selected heart failure patients by improving hemodynamics and functional capacity.
6. Advantages and Limitations
- Advantages:
- Non-invasive and outpatient-based.
- Few adverse effects, typically limited to mild discomfort.
- May serve as an alternative or adjunct therapy for high-risk patients.
- Limitations:
- Effectiveness may vary based on patient-specific factors.
- High costs and limited insurance coverage can restrict accessibility.
- Limited long-term outcome data; more extensive longitudinal studies are needed.
Summary Table of Class Recommendations for EECP in CAD
| Class of Recommendation | Condition | Evidence Level | Rationale |
|---|---|---|---|
| Class IIa | Refractory Angina (not suitable for revascularization) | Strong evidence from studies | Provides symptomatic relief, improves functional capacity, quality of life |
| Class IIb | Coronary Microvascular Dysfunction (CMD) | Limited but emerging evidence | May improve coronary microcirculation, particularly in CMD II trial subjects |
| Class IIb | Heart Failure (selected cases) | Limited observational data | Potential hemodynamic benefits, needs further study |
| Class III | Asymptomatic CAD, or candidates for revascularization | Inadequate benefit or risk | No benefit in asymptomatic cases, risk in patients with specific contraindications |
7. Future Directions
Research on EECP is expanding to include diverse patient populations and various cardiovascular conditions. Advances in imaging and bioengineering are expected to refine EECP protocols, improving efficacy and patient outcomes. Additionally, novel biomarker studies may help tailor EECP therapy to individual patients, ensuring optimal benefit and reducing unnecessary treatments.
8. Conclusion
EECP is a promising and underutilized therapy for CAD, especially beneficial for patients with refractory angina and CMD who are not suitable candidates for revascularization. Ongoing studies continue to clarify its mechanisms and expand its applications in cardiovascular medicine. Future research should focus on long-term efficacy and on exploring EECP’s benefits for broader cardiovascular and systemic health.
References
- Zhang, Y., Chen, J., Yang, D., Yang, Y., Zhong, C., & Wu, G. (2024). Transfer Function Characteristic Analysis of Peripheral Ultrasound Signal Stimulated by Enhanced External Counterpulsation in Patients with Coronary Artery Disease. ResearchSquare. Available at: ResearchSquare PDF
- Cao, F., Liu, Y., Wei, W., & Liang, J. (2024). Effect of enhanced external counterpulsation on coronary microcirculation dysfunction (CMD) in patients with coronary artery disease (EECP-CMD II): study protocol of a randomized controlled trial. BMJ Open, 14(8). Available at: BMJ Open PDF
- Authors. (2022). Enhanced External Counterpulsation Therapy for Refractory Angina: A Review. Cardiovascular Revascularization Medicine, 34, 109-115.